 Below is from a writing assignment from the University of Florida’s Arts in Medicine graduate program.
Below is from a writing assignment from the University of Florida’s Arts in Medicine graduate program.
During my summer practicum in June I worked with Voices of Hope for Aphasia which is a non-profit support group for people with aphasia and their caregivers and family. This is not a group that provides therapy but it does encourage a person with aphasia to practice speaking and feeling confident to carry on a conversation. Aphasia is a language disorder that can affect someone after they have a stroke or serious brain injury. They can be mistaken for someone with a mental or developmental disorder but instead their intellect is intact. It is important for a person with aphasia to feel confident to go out and participate in the world because it will be more difficult to communicate and to be understood.
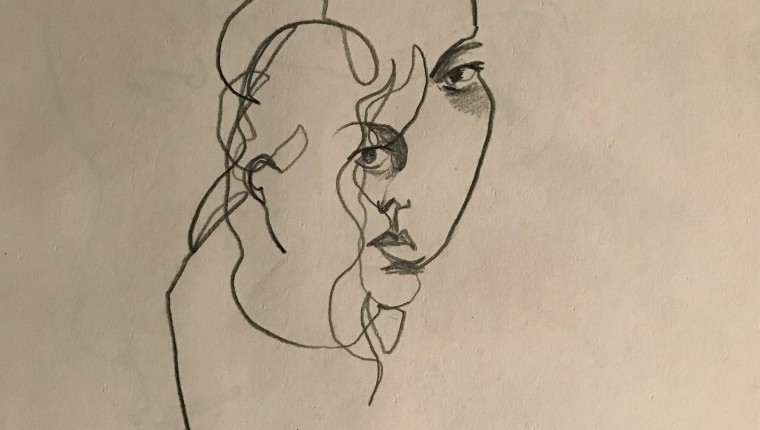
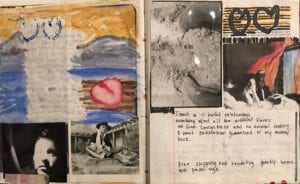
During the month of June it was aphasia awareness month and I wanted to create art projects for the members to express what it feels like to have aphasia to spread awareness of the disorder and the organization. I started out simple by printing out aphasia facts for the members to decorate and personalize so that it was more engaging to look at. The next project was called “what aphasia feels like”. Here I wanted members to visually depict what their brains felt like and what it feels like to speak by drawing in a silhouette of a head and a word bubble on paper. My supervisors loved this project and I spent a great deal of time planning it by prefacing the project with a discussion on abstract expressionists, mark making ideas, and a discussion about depicting feelings. I was so confident in this project I filmed it for my midterm review and sent it in to my advisor.
My advisor alerted me that the project was a little out of my scope of practice as an artist because I was having the members discussing their feelings. In this setting it was difficult for me to determine where the line was that I should not cross as an artist in residence vs. being an art therapist, in which I am not. My advisor explained that because I was asking what the members were feeling, technically that is out of my scope but since my site supervisors had reviewed and asked for me to teach this project then it was acceptable for me to be asking the members of their feelings. She told me of other ways I could rephrase questions about their work like, “can you describe what you created?” “Or why you made a certain mark?” Rather than “what does your brain feel like because you have aphasia?”
My questions are – how do you teach art projects that may ask patients to conjure up feelings and not over step therapeutic boundaries? Is it ever acceptable for an artist in residence to ask a patient to draw a feeling? What if the patient wants to draw their feelings? Do you work with them or do you ask for an art therapist to do the project with the patient? If an art project is going down a very emotional path, what does an artist in residence do if there is no art therapist on hand? Do they stop the project?
I can draw from Florence Nightingale’s writing about giving patients something to view or do to bring them out of the monotony of sickness (Nightingale, 1883). There is a positive impact to wellbeing if a patient feels connected to nature and life instead of removed from it as a patient is confined to a bland existence (Schweitzer, Gilpin, & Frampton, 2004). As I provided a relief from monotony with art project for aphasia members, am I making ethical projects or overstepping boundaries? Hervey explains a nine step process that was developed by Elizabeth Welfel for practitioners to review that can assist in ethical decision making (Hervey, 2007). It summarizes the process that needed to confront ethical dilemmas by acquiring ethical sensitivity, defining the dilemma, reviewing standards and seeking supervisors assistance on your decision made (Hervey, 2007). I experienced this process partially because my ethical sensitivity needs more development as it was brought to my attention that this project may or may not be in my scope of work. Acquiring ethical sensitivity is essential to this profession as well as self-awareness and self-care. From the mythology of Chiron and other wounded healers described in the article by Benziman, we learn that the archetype of this type of healer is also in pain forever because they cannot heal themselves (Benziman, Kannai, & Ahmad, 2012). As artists we must be self-aware and practice self-care because we cannot be the wounded healers in a patient’s life, suffering but still healing others. We cannot sacrifice our lives to heal others because we would be giving nothing in the end.
REFERENCES
Benziman, G., Kannai, R., & Ahmad, A. (2012). The Wounded Healer as Cultural Archetype. CLCWeb: Comparative Literature and Culture, 14(1). https://doi.org/10.7771/1481-4374.1927
Hervey, L.W., (2007). Embodied Ethical Decision Making. American Journal of Dance Therapy.Vol. 29, No. 2. December, 2007.
Nightingale, F. (1883). Notes on nursing : what it is, and what it is not. London : Harrison, 59, Pall Mall, bookseller to the Queen. Retrieved from http://archive.org/details/notesnursingnigh00nigh
Schweitzer, M., Gilpin, L., & Frampton, S. (2004). Healing Spaces: Elements of Environmental Design That Make an Impact on Health. The Journal of Alternative and Complementary Medicine, 10(supplement 1), S-71. https://doi.org/10.1089/acm.2004.10.S-71